Category: Long term care
Millions to lose Medicaid coverage under new law
 Volume 406, Issue 10500
Volume 406, Issue 10500
19 July 2025
WORLD REPORT President Trump’s One Big Beautiful Bill Act makes the largest cuts to Medicaid since its creation, with doctors warning that patients will suffer. Susan Jaffe reports.
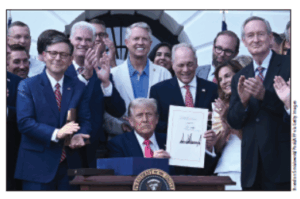
Republicans in the US Congress gave President Donald Trump his first major legislative victory, which provides the largest amount of tax and spending cuts in US history. The One Big Beautiful Bill Act (OBBB) slashes nearly $1 trillion over a decade from Medicaid—the most sweeping cuts since the health insurance programme for people with low incomes was created 60 years ago. The law will hit another historic first by taking health insurance away from more US residents than ever before—nearly 17 million, according to the Congressional Budget Office.
Robert Kennedy Jr’s Promises
 Volume 405, Issue 10480
Volume 405, Issue 10480
1 March 2025
WORLD REPORT To earn enough Senate votes for confirmation as Secretary of the US Department of Health and Human Services (HHS), Robert F Kennedy Jr made some surprising promises for someone aspiring to become the nation’s top health official. He had to reassure a few sceptical Republican senators that he would not overturn years of accepted public health policies, medical practice, and scientific consensus. And yet, in just the short time since assuming his new post on Feb 13, Kennedy’s actions—and inaction—appear to undermine those commitments as thousands of HHS employees are laid off under President Donald Trump’s executive orders shrinking the size and cost of government. [Continued here.]
…
Can the US health-care workforce keep pace with demand?
 Volume 404, Issue 10469
Volume 404, Issue 10469
7 December 2024 
WORLD REPORT A physician and nurse shortage hinders access to care but efforts to educate, recruit, and retain more providers may be threatened. Susan Jaffe reports from Washington, DC.
The uninsured rate in the United States is at an historic low. But a shortage of health-care providers means even people who can afford to go to the doctor might not be able to find one.[Full story here, from The Lancet’s special issue, “A Presidential Briefing Book.”]…
Harris or Trump? Health in the US election
 Volume 404, Issue 10464
Volume 404, Issue 10464
2 November 2024
WORLD REPORT Aside from abortion, health issues have largely been neglected in the run-up to the Nov 5 election. What have the candidates proposed to improve health? Susan Jaffe reports.


As election day approaches on Nov 5, the US presidential race remains a tense and close competition despite unprecedented events—the Democratic candidate was replaced in August, and two attempts have been made to assassinate the Republican candidate. And despite the sharp contrast between former President Donald Trump, a Republican, and Democrat Vice President Kamala Harris, neither has so far managed to emerge as the frontrunner as The Lancet went to press. [Here‘s what the candidates say they would do on abortion, Affordable Care Act and other key health issues.]…
Modest health goals for new US Congress
 Volume 400, Issue 10369
Volume 400, Issue 10369
17 December 2022
WORLD REPORT With Congress almost evenly split between Republicans and Democrats, consensus on any major health legislation is unlikely. Susan Jaffe reports.
When a new US Congress convenes in January, 2023, the slim Republican majority in the House of Representatives and the Democrats’ even smaller margin in the Senate will not enable either party to make major changes in the health-care system. With President Joe Biden promising to use his veto power to defend his health-care agenda, no significant fixes are expected. But there appears to be bipartisan support for some less ambitious legislation on issues that will overcome congressional gridlock.[Continued here.]…
Medicaid Weighs Attaching Strings to Nursing Home Payments to Improve Patient Care
Seeking to Shift Costs to Medicare, More Employers Move Retirees to Advantage Plans
By Susan Jaffe | Kaiser Health News | March 3, 2022 | This KHN story also ran in Fortune and The Dallas Morning News.
…3 States Limit Nursing Home Profits in Bid to Improve Care
“If they choose to rely on public dollars to deliver care, they take on a greater responsibility,” says New York Assemblyman Ron Kim. “It’s not like running a hotel.”
By Susan Jaffe | KAISER HEALTH NEWS | October 25, 2021 | This story also ran on
Nursing homes receive billions of taxpayers’ dollars every year to care for chronically ill frail elders, but until now, there was no guarantee that’s how the money would be spent.
Massachusetts, New Jersey and New York are taking unprecedented steps to ensure they get what they pay for, ![]() after the devastating impact of covid-19 exposed problems with staffing and infection control in nursing homes. The states have set requirements for how much nursing homes
after the devastating impact of covid-19 exposed problems with staffing and infection control in nursing homes. The states have set requirements for how much nursing homes  must spend on residents’ direct care and imposed limits on what they can spend elsewhere, including administrative expenses, executive salaries and advertising and even how much they can pocket as profit. …With this strategy, advocates believe, residents won’t be shortchanged on care, and violations of federal quality standards should decrease because money will be required to be spent on residents’ needs. At least that’s the theory. [Continued on Kaiser Health News, Fortune, NBC News, Yahoo Finance, and Chicago Sun-Times]…
must spend on residents’ direct care and imposed limits on what they can spend elsewhere, including administrative expenses, executive salaries and advertising and even how much they can pocket as profit. …With this strategy, advocates believe, residents won’t be shortchanged on care, and violations of federal quality standards should decrease because money will be required to be spent on residents’ needs. At least that’s the theory. [Continued on Kaiser Health News, Fortune, NBC News, Yahoo Finance, and Chicago Sun-Times]…
The Push For Nursing Home Reform In The Middle Of A Pandemic
 Sept. 20, 2021 | Today on NPR‘s news program “1A,” reporter Susan Jaffe discusses her Kaiser Health News story about new state laws protecting nursing home residents in response to the COVID-19 pandemic. Changes affect staffing, visitation rights, virtual communications, “essential support persons,” and more. A resident of a Connecticut nursing home quoted in this KHN article is also a guest. …
Sept. 20, 2021 | Today on NPR‘s news program “1A,” reporter Susan Jaffe discusses her Kaiser Health News story about new state laws protecting nursing home residents in response to the COVID-19 pandemic. Changes affect staffing, visitation rights, virtual communications, “essential support persons,” and more. A resident of a Connecticut nursing home quoted in this KHN article is also a guest. …
After pandemic ravaged nursing homes, new state laws protect residents
So far, 23 states have passed more than 70 new pandemic-related provisions affecting nursing home operations.
By Susan Jaffe | KAISER HEALTH NEWS | August 17, 2021 | This story also ran in![]()
When the coronavirus hit Martha Leland’s Connecticut nursing home last year, she and dozens of other residents contracted the disease while the facility was on lockdown. Twenty-eight residents died, including her roommate.
“The impact of not having friends and family come in and see us for a year was totally devastating,” she said. “And then, the staff all bound up with the masks and the shields on, that too was very difficult to accept.” She summed up the experience in one word: “scary.”
But under a law Connecticut enacted in June, nursing home residents will be able to designate an “essential support person” who can help

take care of a loved one even during a public health emergency. Connecticut legislators also approved laws this year giving nursing home residents free internet access and digital devices for virtual visits and allowing video cameras in their rooms so family or friends can monitor their care.
Similar benefits are not required by the Centers for Medicare & Medicaid Services, the federal agency that oversees nursing homes and pays for most of the care they provide. But states can impose additional requirements when those federal rules are insufficient or don’t exist. And that’s exactly what many are doing, spurred by the virus that hit the frail elderly hardest. [Continued at Kaiser Health News and USA Today]
…
Chiquita Brooks-LaSure: innovative US federal health director
 Volume 398, Issue 10300
Volume 398, Issue 10300
14 August 2021
PROFILE 
Chiquita Brooks-LaSure, President Joe Biden’s choice to lead the Centers for Medicare and Medicaid Services, presides over an agency with a US$1 trillion budget that provides health insurance to more than 154 million people. Tackling health-care inequities is one of her top priorities. “These disparities have long existed, but COVID-19 has illuminated them in a way that is really unprecedented”, she said. [Full story here.]
…
US FDA defends approval of Alzheimer’s disease drug
 Volume 398, Issue 10294
Volume 398, Issue 10294
3 July 2021
WORLD REPORT An avalanche of criticism has forced the US Food and Drug Administration to defend its decision to grant accelerated approval for aducanumab, the first new Alzheimer’s disease treatment in two decades. “It will be a very long time before we ever figure out whether or not this drug really works”, said Aaron Kesselheim, professor of medicine at Brigham and Women’s Hospital and Harvard Medical School who resigned in protest from an FDA advisory panel that recommended against approval.[Continued here.]
…
Zooming Into the Statehouse: Nursing Home Residents Use New Digital Skills to Push for Changes
By Susan Jaffe | Kaiser Health News | June 9, 2021 | This KHN story also ran on![]() and
and
Patty Bausch isn’t a Medicaid expert, lawyer or medical professional. But she still thinks Connecticut legislators need her input when they consider bills affecting people like her — the roughly 18,000 residents who live in the state’s nursing homes.
With help and encouragement from Connecticut’s Long Term Care Ombudsman Program, Bausch signed up and testified remotely before a legislative hearing this year. Nursing home residents who have been using digital technology to reach out to family and friends — after the covid pandemic led officials to end visitation last year — could also use it to connect with elected officials once the legislature moved to remote hearings. Speaking into an iPad provided by the ombudsman’s office, Bausch testified without ever leaving her room at the Newtown Rehabilitation & Health Care Center, where she has lived since having a stroke three years ago. The combination of a virtual legislature and nursing home residents equipped with internet access has created an opportunity most nursing home residents rarely have — to participate in their government up close and in real time. [Continued on Kaiser Health News, Next Avenue and Connecticut Public Radio.]…
Biden’s first legislative victory: $1·9 trillion for COVID-19
Volume 397, Issue 10279
20 March 2021
WORLD REPORT US President Joe Biden’s first legislative triumph will fund the COVID-19 response and economic recovery, and address social determinants of health. Susan Jaffe reports from Washington, DC.
By narrowly approving a massive COVID-19 response and economic relief package last week, Democrats in Congress handed President Joe Biden his first legislative victory after only 50 days in the White House. The US$1·9 trillion, 628-page, American Rescue Plan Act is a signature achievement so monumental that it has been compared to President Lyndon B Johnson’s sweeping Great Society legislation that raised many Americans out of poverty, with a safety net of social and health services, including the Medicare and Medicaid insurance programmes.
…As the government begins to roll out these benefits, Biden promised “fastidious oversight to make sure there’s no waste or fraud, and the law does what it’s designed to do. And I mean it: we have to get this right… because we have to continue to build confidence in the American people that their government can function for them and deliver.” [Full story with “where the money goes” sidebar here.]
…
What Happens to Nursing Home Workers Who Missed COVID-19 Vaccinations?
COVID-19 has rampaged through nursing homes and other long-term-care facilities, leaving a death toll near 180,000 and counting. So when the first coronavirus vaccines became available at the end of last year, nursing home residents and staff were first in line, given top priority along with emergency responders and health care providers.
![]()
The federal government paid CVS and Walgreens to offer three vaccination clinics for residents and staff at nearly every nursing home in the U.S. That effort, called the Pharmacy Partnership for Long-Term Care Program, wraps up this month. So how do new nursing home residents and workers who missed the onsite clinics get vaccinated now? For residents, plans are in the works to make sure they get the shots. But so far, many of those plans don’t include the staff members who care for them. [Continued here.]…
Nursing Homes Fined for COVID Infection Control Lapses
By Susan Jaffe | Contributing Writer | MedPageToday | November 25, 2020

More than 91,000 residents and staff of long-term care facilities have died after contracting COVID-19 — about 40% of the total deaths in the U.S., according to a Kaiser Family Foundation analysis. …Frustrated by repeated violations of infection control requirements during the pandemic, CMS raised the penalty amounts and announced a crackdown on egregious offenders in August. But the hard-line approach doesn’t seem to have produced the intended results. (Click here for a list of nursing homes that were fined.) [Continued here.]
US Supreme Court poised to keep the Affordable Care Act
Volume 396, Issue 10263
21 November 2020
WORLD REPORT A lawsuit to overturn the Affordable Care Act may be floundering after Supreme Court justices questioned why the law should be dismantled. Susan Jaffe reports from Washington, DC.
The fate of the Affordable Care Act (ACA) is again in the hands of the US Supreme Court, after close calls in lawsuits in 2012 and 2015. But last week’s hearing was different: justices who once voted to overturn the law— along with President Donald Trump’s recent court appointees—bombarded opponents with sceptical questions.
After oral arguments in the case, known as California v. Texas, legal experts believe President Barack Obama’s signature health reform law is not in mortal danger. [Continued here.]
…US election 2020: the future of the Affordable Care Act
Volume 396, Number 10260 31 October 2020
WORLD REPORT President Donald Trump pledges to replace the Affordable Care Act while his Democratic opponent Joe Biden offers detailed proposals to improve it. Susan Jaffe reports from Washington, DC.
Since winning the presidency in 2016 in large part by promising to eliminate Obamacare, otherwise known as the Affordable Care Act (ACA), Donald Trump has promised more than a dozen times that his replacement plan would be ready soon. The plan would be released in 2 weeks, a White House spokeswoman said 2 months ago.

“We’re going to have a health-care plan that will be second to none”, Trump said in 2017. “It’s going to be great and the people will see that.” And at last week’s final presidential debate, he vowed “to terminate Obamacare, [and] come up with a brand new beautiful health care”.
A decade after the ACA—President Barack Obama’s signature achievement—became law, repealing and replacing Obamacare is again central to Trump’s re-election. And improving and expanding the law is a crucial part of the campaign of his challenger, former Vice President Joe Biden. [Continued here.]
…Pandemic Deals Another Blow To Nursing Homes: Plummeting Occupancy
BY SUSAN JAFFE | CONNECTICUT HEALTH INVESTIGATIVE TEAM | SEPTEMBER 16, 2020 
While the deadly coronavirus seems to be subsiding in Connecticut for now, its impact on nursing homes has not. More than 6,700 beds are empty, and it may take many months of financial struggle before occupancy climbs back to pre-pandemic levels.
Of the approximately 200 nursing homes in Connecticut that receive payments from Medicaid, the government health insurance program for low-income people, only 15 were
70% or less occupied in January, according to the Connecticut Health Investigative Team’s analysis of state data. By August, almost five times as many facilities saw occupancy drop to that level or less….
Owners say the state and federal governments aren’t doing enough to shore up their industry and protect residents during the pandemic. And in some cases, policies intended to control the virus can make things worse. [Continued here, with map and table of dangerously low occupancy nursing homes.]…
CMS Warns of COVID-19 Spike in Nursing Homes
Medicare chief says “significant deficiencies in infection control practices” in nursing homes have doubled weekly COVID-19 cases, but “this isn’t a time of fines and being punitive.”
Whether By Luck Or Safety Protocols, Some Nursing Homes Remain COVID-19 Free
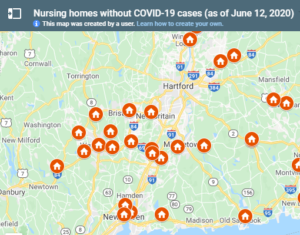
BY SUSAN JAFFE | CONNECTICUT HEALTH INVESTIGATIVE TEAM | JUNE 15,2020 
The coronavirus has decimated many of the nation’s nursing homes, and elderly, chronically ill residents of these facilities account for 64% of the state’s 4,201 death toll. They are roughly 100 times more likely to die of the virus than other people in the state.
So, the fact that some 41 of Connecticut’s 214 nursing homes have managed to keep out the virus, according to an analysis by C-HIT, is both remarkable and mystifying. Did they just get lucky?
Administrators at several COVID-19-free facilities use the word “fortunate” to describe a situation they acknowledge could change at any time. [Continued here, with map and table of COVID-19 free nursing homes.]
…Hundreds Died of COVID at NYC Nursing Homes With Spotless Infection Inspections
By Susan Jaffe | THE CITY | May 27, 2020 
More than 600 residents have died from COVID-19 at 25 New York City nursing homes that received clean bills of health for controlling the spread of infections, state Department of Health inspection reports obtained by THE CITY show.
Those facilities inclu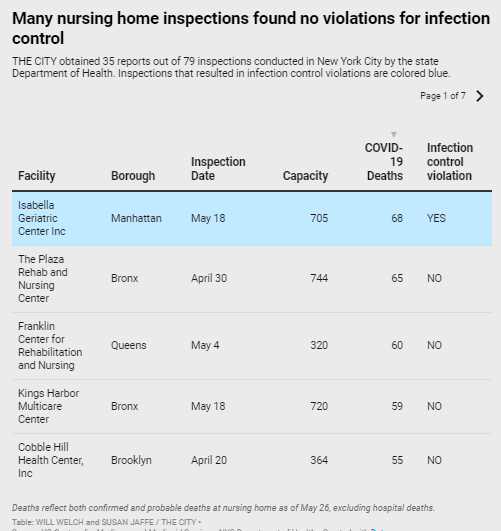 de homes with some of the highest coronavirus death tolls in the nation — including the Sapphire Center for Rehabilitation and Nursing in Flushing, which reports 54 residents died of confirmed or presumed COVID….
de homes with some of the highest coronavirus death tolls in the nation — including the Sapphire Center for Rehabilitation and Nursing in Flushing, which reports 54 residents died of confirmed or presumed COVID….
At the Franklin Center for Rehabilitation and Nursing, also in Flushing, 60 residents — nearly one in five — succumbed to the virus. Its May 4 inspection report found no problems.
Also passing its May 11 infection-control inspection was New York State Veterans Home in St. Albans, Queens. Staff there previously told THE CITY that the state Health Department-run home failed to separate COVID-positive and uninfected residents, something that was a violation at other facilities….
“It’s very shocking that at the apex of this pandemic, our inspectors went in and reported that that there’s nothing out of the ordinary when it’s clear that the infection rate had spread,” said Assemblymember Ron Kim (D-Queens), whose district includes Sapphire and the Franklin Center. [continued here].
…As Congress Weighs COVID Liability Protections, States Shield Health Providers
By Susan Jaffe | Kaiser Health News | May 14, 2020 | This story also ran on 
Coronavirus patients and their families who believe a doctor, nurse, hospital or other provider made serious mistakes during their care may face a new hurdle if they try to file medical malpractice lawsuits.
Under pressure from health provider organizations, governors in Connecticut, Maryland, Illinois and several other states have ordered that most providers be shielded from civil ― and, in some cases, criminal— lawsuits over medical treatment during the C OVID-19 health emergency. In New York and New Jersey, immunity is now part of state law….
Some legal experts and seniors’ advocates worry that the state immunity guarantees go too far, leaving patients with no way to hold providers accountable. Supporters argue that health care providers and facilities deserve protection from lawsuits as they battle a deadly virus during an unprecedented public health emergency. [Continued at Kaiser Health News and Daily Beast. ]
…Nursing Home Watchdogs Scarce At NYC Facilities As Hundreds Die Within
CLOSED DOORS | THE CITY | April 23, 2020
By

Eyes and ears usually trained on New York’s nursing homes and adult care facilities have been nearly locked out as the coronavirus has claimed the lives of more than 3,500 residents statewide.

Almost entirely out of the picture are nursing home inspectors,employed by the state Department of Health and
coordinated by the federal government, who are responsible for ensuring that the facilities comply with federal health and safety requirements.
“Nursing facilities are essentially free of public scrutiny right now, at a time when scrutiny is more important than ever,” said Susan Dooha, executive director of the Center for Independence of the Disabled in New York [continued here].
…