 Volume 400, Issue 10365
Volume 400, Issue 10365
19 November 2022
WORLD REPORT An independent review made several recommendations for improving the public health agency. Susan Jaffe reports from Washington, DC.
 Volume 400, Issue 10365
Volume 400, Issue 10365
WORLD REPORT An independent review made several recommendations for improving the public health agency. Susan Jaffe reports from Washington, DC.

 Volume 400, Issue 10362
Volume 400, Issue 10362
WORLD REPORT Makena has been given to hundreds of thousands of patients over the past 11 years. Susan Jaffe reports from Washington, DC.
The only treatment in the USA to prevent premature births is ineffective and should be withdrawn from the market, according to the Food and Drug Administration’s (FDA) Obstetrics, Reproductive and Urologic Drug Advisory Committee. The recommendation has renewed scrutiny of a special drug approval process that raises patients’ hopes by allowing them to take medications that have not been fully tested for efficacy and safety [Continued here.]
 Volume 400, Issue 10354
Volume 400, Issue 10354
WORLD REPORT The recently passed Inflation Reduction Act will provide billions of dollars of incentives to reduce greenhouse gas emissions. Susan Jaffe reports.
There are no emission limits or pollution penalties in the landmark Inflation Reduction Act that Congress approved in August. Instead of forcing cuts, the climate change and healthcare law provides US$370 billion worth of incentives to ratchet down the planet-warming greenhouse gases from fossil fuels that have caused record-breaking heat waves, wild fires, droughts, and floods. …The law provides $60 billion for communities that have been disproportionately affected by toxic hazards and the consequences of climate change. [Continued here.]
 Volume 400, Issue 10352
Volume 400, Issue 10352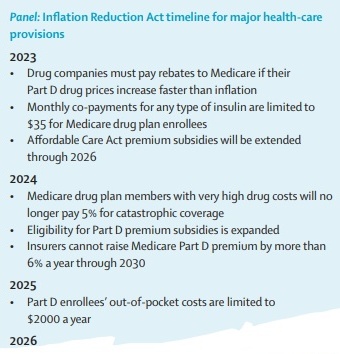
WORLD REPORT A new law also targets climate change in a major victory for Democrats and President Joe Biden. Susan Jaffe reports from Washington, DC.
 Volume 400, Issue 10346
Volume 400, Issue 10346
WORLD REPORT A patchwork of state laws replace abortion rights once guaranteed by Roe v Wade. Susan Jaffe reports from Washington, DC.
 Volume 400, Issue 10345
Volume 400, Issue 10345
2 July 2022
WORLD REPORT The US Supreme Court’s decision to overturn Roe v Wade is due to spark further court cases. Susan Jaffe reports from Washington, DC.
 Volume 399, Issue 10347
Volume 399, Issue 10347
WORLD REPORT Both Republican and Democrat legislators have called for changes following a shortage of breastmilk substitute. Susan Jaffe reports from Washington, DC..
The leading US producer of infant formula resumed partial operations on June 4 following a 4-month shutdown, but it may take several more weeks before supplies return to normal, along with the shortage-induced panic and desperation of American parents. When the US Food and Drug Administration (FDA) can regain trust in its ability to police the nation’s food manufacturers is another matter.
The agency’s failure to respond quickly to health hazards at the Abbott Nutrition facility in Sturgis, MI, that released potentially contaminated formula across the country has provoked rare bipartisan outrage in Congress and equally rare apologies from the manufacturer. The shutdown and resulting shortage have also prompted calls for major changes in the FDA’s food safety division, along with questions about why one supplier dominates the market. [Continued here.]

In February, 2022, US President Joe Biden appointed global health physician and epidemiologist Raj Panjabi as a Special Assistant to the President and Senior Director for Global Health Security and Biodefense at the White House National Security Council in Washington, DC, which advises Biden on foreign policy and security issues.[Continued here.]
 Volume 399, Issue 10338
Volume 399, Issue 10338
WORLD REPORT Health and human rights groups are concerned that many states would outlaw abortion if the Supreme Court topples Roe v Wade. Susan Jaffe reports.
Protests and celebrations erupted across the USA following the unprecedented leak of a draft Supreme Court decision that would overturn the court’s 1973 landmark Roe v Wade ruling establishing a woman’s right to a safe and legal abortion. …“States are already working together to create enormous abortion deserts that many people will not be able to cross”, said Nancy Northup, president and CEO of the Center for Reproductive Rights. [Continued here.]
 Volume 399, Issue 10335
Volume 399, Issue 10335
WORLD REPORT The federal health plan for older Americans will pay for the controversial new drug aducanumab only for patients participating in clinical trials. Susan Jaffe reports.