By
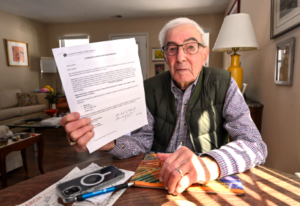
Ever since Larry Wilkewitz retired more than 20 years ago from a wood products company, he’s had a commercial Medicare Advantage plan from the insurer Humana.
But two years ago, he heard about Peak Health, a new Advantage plan started by the West Virginia University Health System, where his doctors practice. It was cheaper and offered more personal attention, plus extras such as an allowance for over-the-counter pharmacy items. Those benefits are more important than ever, he said, as he’s treated for cancer.
“I decided to give it a shot,” said Wilkewitz, 79. “If I didn’t like it, I could go back to Humana or whatever after a year.” He’s sticking with Peak Health. Members of Medicare Advantage plans, a privately run alternative to the government’s Medicare program, can change plans through the end of March.
…Although hospital-owned plans are only a sliver of the Medicare Advantage market, their enrollment continues to grow, reflecting the overall increase in Advantage members. Of the 62.8 million Medicare beneficiaries eligible to join Advantage plans, 54% signed up last year, according to KFF, the health information nonprofit that includes KFF Health News. While the number of Advantage plans owned by hospital systems is relatively stable, Mass General Brigham in Boston and others are expanding their service areas and types of plan offerings.
… Medicare Advantage plans usually restrict their members to a network of doctors, hospitals, and other clinicians that have contracts with the plans to serve them. But if hospitals and plans can’t agree to renew those contracts, or when disputes flare up — often spurred by payment delays, denials, or burdensome prior authorization rules — the health care providers can drop out. These break-ups, plus planned terminations and service area cuts, forced more than 3.7 million Medicare Advantage enrollees to make a tough choice last year: find new insurance for 2026 that their doctors accept or, if possible, keep their plan but find new doctors.[Continued on KFF Health News, US News & World Report, Modern Healthcare, Medpage Today, and Fierce Health.]






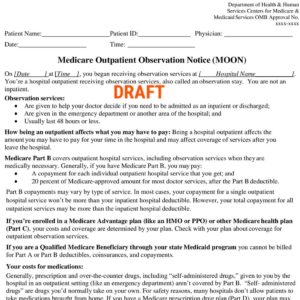 was a response to complaints from Medicare patients who were surprised to learn that although they had spent a few days in the hospital, they were there for observation and were not admitted. Observation patients are considered too sick to go home yet not sick enough to be admitted. They may pay higher charges than admitted patients and do not qualify for Medicare’s nursing home coverage.
was a response to complaints from Medicare patients who were surprised to learn that although they had spent a few days in the hospital, they were there for observation and were not admitted. Observation patients are considered too sick to go home yet not sick enough to be admitted. They may pay higher charges than admitted patients and do not qualify for Medicare’s nursing home coverage.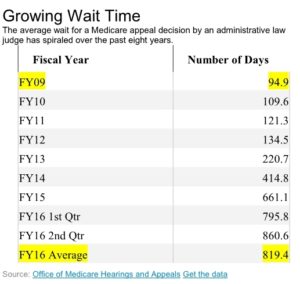 challenging denied claims continues to spiral, increasing the backlog of cases and delaying many decisions well beyond the timeframes set by law, according to a government study released Thursday.
challenging denied claims continues to spiral, increasing the backlog of cases and delaying many decisions well beyond the timeframes set by law, according to a government study released Thursday.