 Volume 400, Issue 10365
Volume 400, Issue 10365
19 November 2022
WORLD REPORT An independent review made several recommendations for improving the public health agency. Susan Jaffe reports from Washington, DC.
 Volume 400, Issue 10365
Volume 400, Issue 10365
WORLD REPORT An independent review made several recommendations for improving the public health agency. Susan Jaffe reports from Washington, DC.
So far, 23 states have passed more than 70 new pandemic-related provisions affecting nursing home operations.
By Susan Jaffe | KAISER HEALTH NEWS | August 17, 2021 | This story also ran in![]()
When the coronavirus hit Martha Leland’s Connecticut nursing home last year, she and dozens of other residents contracted the disease while the facility was on lockdown. Twenty-eight residents died, including her roommate.
“The impact of not having friends and family come in and see us for a year was totally devastating,” she said. “And then, the staff all bound up with the masks and the shields on, that too was very difficult to accept.” She summed up the experience in one word: “scary.”
But under a law Connecticut enacted in June, nursing home residents will be able to designate an “essential support person” who can help

take care of a loved one even during a public health emergency. Connecticut legislators also approved laws this year giving nursing home residents free internet access and digital devices for virtual visits and allowing video cameras in their rooms so family or friends can monitor their care.
Similar benefits are not required by the Centers for Medicare & Medicaid Services, the federal agency that oversees nursing homes and pays for most of the care they provide. But states can impose additional requirements when those federal rules are insufficient or don’t exist. And that’s exactly what many are doing, spurred by the virus that hit the frail elderly hardest. [Continued at Kaiser Health News and USA Today]
…
 Volume 398, Issue 10300
Volume 398, Issue 10300

…
By Susan Jaffe | Contributing Writer | MedPageToday | November 25, 2020

More than 91,000 residents and staff of long-term care facilities have died after contracting COVID-19 — about 40% of the total deaths in the U.S., according to a Kaiser Family Foundation analysis. …Frustrated by repeated violations of infection control requirements during the pandemic, CMS raised the penalty amounts and announced a crackdown on egregious offenders in August. But the hard-line approach doesn’t seem to have produced the intended results. (Click here for a list of nursing homes that were fined.) [Continued here.]

More than 600 residents have died from COVID-19 at 25 New York City nursing homes that received clean bills of health for controlling the spread of infections, state Department of Health inspection reports obtained by THE CITY show.
Those facilities inclu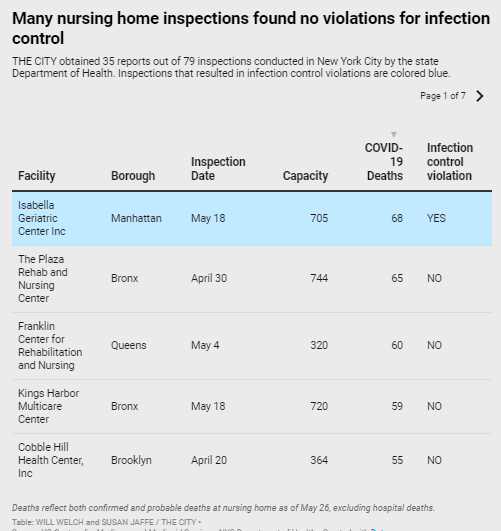 de homes with some of the highest coronavirus death tolls in the nation — including the Sapphire Center for Rehabilitation and Nursing in Flushing, which reports 54 residents died of confirmed or presumed COVID….
de homes with some of the highest coronavirus death tolls in the nation — including the Sapphire Center for Rehabilitation and Nursing in Flushing, which reports 54 residents died of confirmed or presumed COVID….
At the Franklin Center for Rehabilitation and Nursing, also in Flushing, 60 residents — nearly one in five — succumbed to the virus. Its May 4 inspection report found no problems.
Also passing its May 11 infection-control inspection was New York State Veterans Home in St. Albans, Queens. Staff there previously told THE CITY that the state Health Department-run home failed to separate COVID-positive and uninfected residents, something that was a violation at other facilities….
“It’s very shocking that at the apex of this pandemic, our inspectors went in and reported that that there’s nothing out of the ordinary when it’s clear that the infection rate had spread,” said Assemblymember Ron Kim (D-Queens), whose district includes Sapphire and the Franklin Center. [continued here].
…The FDA’s emergency use authorisation (EUA) issued last week gives physicians the option to prescribe the drugs, which President Donald Trump has recommended. However, both drugs are unproven and untested for COVID-19, and have rare but potentially deadly side-effects. The decision bypassed the usual drug approval process including doubleblind, placebo-controlled clinical trials, stoking a worldwide debate about whether the drugs are appropriate for treating the disease.
“I think it was resorted to more out of a sense of desperation”, said Joseph Masci, an infectious disease specialist and director of global health at Elmhurst Hospital in Queens, a borough of New York City, which is at the centre of the epidemic in the USA. “It is just an indication of how sudden and massive this outbreak has been.” [Continued here.]
…