By ,
This article also ran in The Washington Post.
Judith Sullivan was recovering from major surgery at a Connecticut nursing home in March when she got surprising news from h when she got surprising news from her Medicare Advantage plan: It would no longer pay for her care because she was well enough to go home.
At the time, she could not walk more than a few feet, even with assistance — let alone manage the stairs to her front door, she said. She still needed help using a colostomy bag following major surgery.
“How could they make a decision like that without ever coming and seeing me?” said Sullivan, 76. “I still couldn’t walk without one physical therapist behind me and another next to me. Were they all coming home with me?” 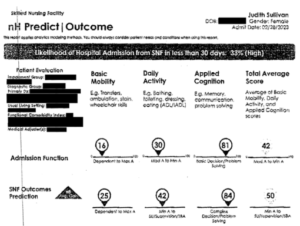
UnitedHealthcare — the nation’s largest health insurance company, which provides Sullivan’s Medicare Advantage plan — doesn’t have a crystal ball. It does have naviHealth, a care management company bought by UHC’s sister company, Optum, in 2020. NaviHealth’s proprietary “nH Predict” tool sifts through millions of medical records to match patients with similar diagnoses and characteristics, including age, preexisting health conditions, and other factors. Based on these comparisons, an algorithm anticipates what kind of care a specific patient will need and for how long.
…Next year, the Centers for Medicare & Medicaid Services will begin restricting how Medicare Advantage plans use predictive technology tools to make some coverage decisions.[Continued on Kaiser Health News and The Washington Post.]…

