By Susan Jaffe | Kaiser Health News | August 12, 2019 | This KHN story also ran on Salon and Next Avenue
Medicare paid for Betty Gordon’s knee replacement surgery in March, but the 72-year-old former high school teacher needed a nursing home stay and care at home to recover.

Yet Medicare wouldn’t pay for that. So Gordon is stuck with a $7,000 bill she can’t afford — and, as if that were not bad enough, she can’t appeal.

The reasons Medicare won’t pay have frustrated the Rhode Island woman and many others trapped in the maze of regulations surrounding something called “observation care.”
Patients, like Gordon, receive observation care in the hospital when their doctors think they are too sick to go home but not sick enough to be admitted. They stay overnight or longer, usually in regular hospital rooms, getting some of the same services and treatment (often for the same problems) as an admitted patient….

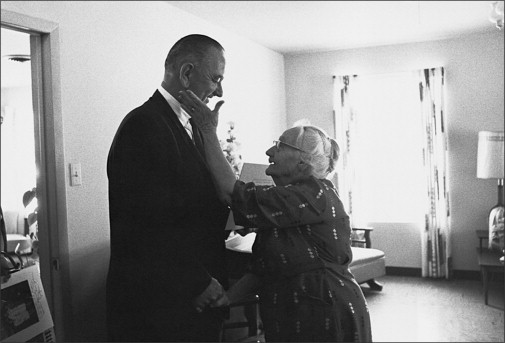
(Photo courtesy of Betty Gordon)
But observation care is considered an outpatient service under Medicare rules, like a doctor’s appointment or a lab test. Observation patients may have to pay a larger share of the hospital bill than if they were officially admitted to the hospital.Medicare’s nursing home benefit is available only to those admitted to the hospital for three consecutive days. Gordon spent three days in the hospital after her surgery, but because she was getting observation care, that time didn’t count.

There’s another twist: Patients might want to file an appeal, as they can with many other Medicare decisions. But that is not allowed if the dispute involves observation care.
Monday, a trial begins in federal court in Hartford, Conn., where patients who were denied Medicare’s nursing home benefit are hoping to force the government to eliminate that exception. A victory would clear the way for appeals from hundreds of thousands of people. [Continued at Kaiser Health News, Next Avenue or Salon]
…




 For years, most pharmacists couldn’t give customers even a clue about an easy way to save money on prescription drugs. But the restraints are coming off.
For years, most pharmacists couldn’t give customers even a clue about an easy way to save money on prescription drugs. But the restraints are coming off.
 period for these private drug and Advantage plans for 2016 starts Thursday and runs through Dec. 7.
period for these private drug and Advantage plans for 2016 starts Thursday and runs through Dec. 7.
 e the Affordable Care Act, older adults who couldn’t afford to buy their own health insurance would count the days until their 65th birthday, when Medicare would kick in. Now, 10,000 Americans hit that milestone every day, but for some who have coverage through the ACA’s insurance marketplaces, Medicare may not be the obvious next step.
e the Affordable Care Act, older adults who couldn’t afford to buy their own health insurance would count the days until their 65th birthday, when Medicare would kick in. Now, 10,000 Americans hit that milestone every day, but for some who have coverage through the ACA’s insurance marketplaces, Medicare may not be the obvious next step.

 switch out of their plans and join traditional Medicare or another Medicare Advantage plan whose provider network includes their doctors.
switch out of their plans and join traditional Medicare or another Medicare Advantage plan whose provider network includes their doctors.
 A disabled senior with serious health problems who successfully challenged Medicare for denying her home health care coverage has racked up another win against the government.
A disabled senior with serious health problems who successfully challenged Medicare for denying her home health care coverage has racked up another win against the government. “I’m very pleased. It makes me feel America is still in good shape.”
“I’m very pleased. It makes me feel America is still in good shape.” 
 smoking. The doctor said Medicare would cover the procedure. So Driscoll, 68, who lives in Silver Spring, had the test done and was surprised when he got a bill from Medicare for $214.
smoking. The doctor said Medicare would cover the procedure. So Driscoll, 68, who lives in Silver Spring, had the test done and was surprised when he got a bill from Medicare for $214.
 But officials looking for ways to cut the federal deficit are suggesting that these Medigap policies help explain why the government’s Medicare bill is rising so fast. If these private policies were less generous, they figure, seniors might reduce their trips to the doctor or find cheaper care, which in turn would save the government money.Fisher, 86, a cancer survivor from Gaithersburg who has had two hip replacements, says that strategy could backfire… [Continued on
But officials looking for ways to cut the federal deficit are suggesting that these Medigap policies help explain why the government’s Medicare bill is rising so fast. If these private policies were less generous, they figure, seniors might reduce their trips to the doctor or find cheaper care, which in turn would save the government money.Fisher, 86, a cancer survivor from Gaithersburg who has had two hip replacements, says that strategy could backfire… [Continued on 
