Tag: observation care
Under New Cost-Cutting Medicare Rule, Same Surgery, Same Place, Different Bill
By Susan Jaffe | Kaiser Health News | March 21, 2021 | This KHN story also ran in The Washington Post
For years, Medicare officials considered some su rgeries so risky for older adults that that the insurance program would cover the procedures only for patients admitted to the hospital. Under a new Medicare policy that took effect this year, these operations can be provided to patients who are not admitted. But patients still have to go to the hospital. The change saves Medicare money while patients can pay a larger share of the bill — for the same surgery at the same hospital. [Full story in The Washington Post and Kaiser Health News.]
rgeries so risky for older adults that that the insurance program would cover the procedures only for patients admitted to the hospital. Under a new Medicare policy that took effect this year, these operations can be provided to patients who are not admitted. But patients still have to go to the hospital. The change saves Medicare money while patients can pay a larger share of the bill — for the same surgery at the same hospital. [Full story in The Washington Post and Kaiser Health News.]
… CMS lost $84M in two years for ineligible nursing home stays
IG investigators said such improper payments are accumulating year after year.

By Susan Jaffe | Modern Healthcare | February 20, 2019
The CMS pays millions of dollars a year to nursing homes for taking care of older adults who don’t qualify for coverage, according to an investigation by HHS’ inspector general.
The IG’s report, released Wednesday, includes steps the CMS should take to fix the problem; but in a written response, CMS Administrator Seema Verma rejected some key recommendations. [Continued here.]…
By Law, Hospitals Now Must Tell Medicare Patients When Care Is ‘Observation’ Only
By Susan Jaffe | KAISER HEALTH NEWS | March 13, 2017 |This story also ran in 
Under a new federal law, hospitals across the country must now alert Medicare patients when they are getting observation care and why they were not admitted — even if they stay in the hospital a few nights. For years, seniors often found out only when they got
surprise bills for the services Medicare doesn’t cover for observation patients, including some drugs and expensive nursing home care.
The notice may cushion the shock but probably not settle the issue.
When patients are too sick to go home but not sick enough to be admitted, observation care gives doctors time to figure out what’s wrong. It is considered an outpatient service, like a doctor’s visit. Unless their care falls under a new Medicare bundled-payment category, observation patients pay a share of the cost of each test, treatment or other services. And if they need nursing home care to recover their strength, Medicare won’t pay for it because that coverage requires a prior hospital admission of at least three consecutive days.
Observation time doesn’t count.
“Letting you know would help, that’s for sure,” said Suzanne Mitchell, of Walnut Creek, Calif. When her 94-year-old husband fell and was taken to a hospital last September, she was told he would be admitted. It was only after seven days of hospitalization that she learned he had been an observation patient. He was due to leave the next day and enter a nursing home, which Medicare would not cover. She still doesn’t know why.
“If I had known [he was in observation care], I would have been on it like a tiger because I knew the consequences
by then, and I would have done everything I could to insist that they change that outpatient/inpatient,” said Mitchell, a retired respiratory therapist. “I have never, to this day, been able to have anybody give me the written policy the hospital goes by to decide.” Her husband was hospitalized two more times and died in December. His nursing home sent a bill for nearly $7,000 that she has not yet paid. [Continued at Kaiser Health News and USA Today] …
Medicare Releases Draft Proposal For Patient Observation Notice
By Susan Jaffe | KAISER HEALTH NEWS | June 15, 2016 |This story also ran in 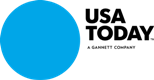
In just two months, a federal law kicks in requiring hospitals to tell their Medicare patients if they have not been formally admitted and why. But some physician, hospital and consumer representatives say a notice drafted by Medicare for hospitals to use may not do the job.
The law was a response to complaints from Medicare patients who were surprised to learn that although they had spent a few days in the hospital, they were there for observation and were not admitted. Observation patients are considered too sick to go home yet not sick enough to be admitted. They may pay higher charges than admitted patients and do not qualify for Medicare’s nursing home coverage.
was a response to complaints from Medicare patients who were surprised to learn that although they had spent a few days in the hospital, they were there for observation and were not admitted. Observation patients are considered too sick to go home yet not sick enough to be admitted. They may pay higher charges than admitted patients and do not qualify for Medicare’s nursing home coverage.
The NOTICE Act requires that starting Aug. 6, Medicare patients receive a form written in “plain language” after 24 hours of observation care but no later than 36 hours. Under the law, it must explain the reason they have not been admitted and how that decision will affect Medicare’s payment for services and patients’ share of the costs. The information must also be provided verbally, and a doctor or hospital staff member must be available to answer questions
And patients could have questions, said Brenda Cude, a National Association of Insurance Commissioners consumer representative and professor of consumer economics at the University of Georgia. She said the notice is written for a 12th-grade reading level, even though most consumer materials aim for no more than an eighth-grade level. It “assumes some health insurance knowledge that we are fairly certain most people don’t have.”
…The form does not meet the expectations of Rep. Lloyd Doggett, D-Texas, who co-sponsored the law. “I am concerned that the proposed notice fulfills neither the spirit nor the letter of the law,” Doggett said in an interview. [Continuted at Kaiser Health News or USA Today]…
Congress Overwhelmingly Approves Bill Bolstering Medicare Patients’ Hospital Rights
By Susan Jaffe | Kaiser Health News | July 29, 2015 | This KHN story also ran in 
The U.S. Senate unanimously approved legislation Monday night requiring hospitals across the nation to tell Medicare patients when they receive observation care but have not been admitted to the hospital. It’s a distinction that’s easy to miss until patients are hit with big medical bills after a short stay.
miss until patients are hit with big medical bills after a short stay.
The vote follows overwhelming approval in the U. S. House of Representatives in March. The legislation is expected to be signed into law by President Barack Obama, said its House sponsor, Texas Democratic Rep. Lloyd Doggett.
It’s called the NOTICE Act, short for “Notice of Observation Treatment and Implication for Care Eligibility.” The law would require hospitals to provide written notification to patients 24 hours after receiving observation care, explaining that they have not been admitted to the hospital, the reasons why, and the potential financial implications.
Those implications can be dire. Observation care hurts seniors in two ways: It keeps Medicare’s more comprehensive hospitalization coverage from kicking in, and it means they may not get Medicare’s limited nursing home benefit if they need care in a facility after being in a hospital.
To qualify for Medicare’s nursing home coverage, beneficiaries must first spend three consecutive midnights as an admitted patient in a hospital, and observation days don’t count. Without that coverage, seniors could pay thousands of dollars for the nursing home care their doctor ordered, or else try to recover on their own. Observation care is a classification used when patients are not well enough to go home but not sick enough to be admitted. [Continued in Kaiser Health News]…
Seniors’ Wait For A Medicare Appeal Is Cut In Half
By Susan Jaffe KAISER HEALTH NEWS | December 23, 2014
The federal office responsible for appeals for Medicare coverage has cut in half the waiting time for beneficiaries who are requesting a hearing before a judge.
The progress follows an announcement last January that officials were going to work through a crushing backlog by moving beneficiaries to the front of the line and suspending hearings on cases from hospitals, doctors and other providers for at least two years.
…Still, about 900,000 appeals are awaiting decisions, with most filed by hospitals, nursing homes, medical device suppliers and other health care providers, said Jason Green, OMHA’s program and policy director. The wait times for health providers’ cases have doubled since last year, and are nearly four times longer than the processing time for beneficiary appeals. [Continued in KHN] [Continued in Washington Post]…
Hospitals Required To Tell Patients Of Observation Care Status
By Susan Jaffe | September 30, 2014
Connecticut Health Investigative Team and The Hartford Courant
Starting Wednesday, a new state law requires Connecticut hospitals to tell all patients when ![]() they are being kept in the hospital for observation instead of being admitted and to warn them about the financial consequences.
they are being kept in the hospital for observation instead of being admitted and to warn them about the financial consequences.
Anyone who goes to the hospital can be placed on observation status, so that doctors can determine what’s wrong, and decide whether the patient is sick enough to be admitted or well enough to go home. Observation patients may receive diagnostic tests, medications, some treatment, and other outpatient services. Depending on their insurance, they can be  charged a share of the cost. In addition to hospital bills, Medicare observation patients whose doctors order follow-up nursing home care will have to pay the nursing home themselves. Medicare covers nursing homes only after seniors are admitted to the hospital and stay through three consecutive midnights. A month in a Connecticut nursing home can cost as much as $15,000.
charged a share of the cost. In addition to hospital bills, Medicare observation patients whose doctors order follow-up nursing home care will have to pay the nursing home themselves. Medicare covers nursing homes only after seniors are admitted to the hospital and stay through three consecutive midnights. A month in a Connecticut nursing home can cost as much as $15,000.
Medicare does not require hospitals to tell patients when they are getting observation care and what it means. And the number of Medicare observation patients is growing rapidly — 88 percent in the past six years, to 1.8 million nationally in 2012, according to the Medicare Payment Advisory Commission, an independent government agency.
…Meanwhile, more states are trying to address the situation. Connecticut becomes at least the third state in the nation, after New York and Maryland to require notification for observation status. Massachusetts, New Jersey and Pennsylvania are considering similar laws. CONTINUED in Connecticut Health Investigative Team CONTINUED in The Courant …
Medicare Testing Payment Options That Could End Observation Care Penalties
By Susan Jaffe KAISER HEALTH NEWS | July 22, 2014 | This KHN story also ran in ![]()
Medicare officials have allowed patients at dozens of hospitals participating in pilot projects across the country to be exempted from the controversial requirement that limits nursing home coverage to seniors admitted to a hospital for at least three days.
The idea behind these experiments is to find out whether new payment arrangements with the hospitals and other health care providers that drop the three-day rule can reduce costs or keep them the same while improving the quality of care. They are conducted under a provision of the Affordable Care Act that created the Center for Medicare and Medicaid Innovations to develop ways of improving Medicare.
If the experiment saves Medicare money and improves care, “we should be able to make an argument to Medicare that there is a way to do it for all our patients,” said Dr. Eric Weil, clinical affairs associate chief for the general internal medicine division at Massachusetts General Hospital in Boston. The hospital is one of five in the Partners Health System that began offering the waiver in April, after testing a limited version.
“It gets patients to the care they need much quicker and prevents them from clinically declining at home,” said Weil. If patients can spend less time in the hospital, he said that frees up valuable resources for sicker patients. And it saves money for Medicare because nursing home care or home health care is cheaper than a hospital stay. [Continued in KHN] [Continued in Washington Post]…
FAQ: Hospital Observation Care Can Be Costly For Medicare Patients
By Susan Jaffe | UPDATED June 18, 2014 | KAISER HEALTH NEWS ![]()
Some seniors think Medicare made a mistake. Others are just stunned when they find out that being in a hospital for days doesn’t always mean they were actually admitted.
Instead, they received observation care, considered by Medicare to be an outpatient service. Yet, a recent government investigation found that observation patients often have the same health problems as those who are admitted. But the observation designation means they can have higher out-of-pocket expenses and fewer Medicare benefits. Here are some common questions and answers about observation care and the coverage gap that can result. [MORE] …
Medicare May Be Overpaying Hospitals For Patients Who Don’t Stay Long
By Susan Jaffe | Kaiser Health News in collaboration with National Public Radio | May 21, 2014, 9:35 a.m.
 The federal government may be paying hospitals $5 billion too much as a result of an 18-month moratorium on enforcement of Medicare rules that tell hospitals when patients should be admitted, an independent Medicare auditing company told a congressional panel yesterday. The controversial rules were intended to reduce the increasing number of seniors hospitalized for observation but not admitted. If they have not been admitted to the hospital for at least three consecutive days, they are not eligible for follow-up nursing home coverage and may have higher out-of-pocket expenses while in the hospital. Medicare pays hospitals more for admitted patients than observation patients. MORE from NPR and Kaiser Health News …
The federal government may be paying hospitals $5 billion too much as a result of an 18-month moratorium on enforcement of Medicare rules that tell hospitals when patients should be admitted, an independent Medicare auditing company told a congressional panel yesterday. The controversial rules were intended to reduce the increasing number of seniors hospitalized for observation but not admitted. If they have not been admitted to the hospital for at least three consecutive days, they are not eligible for follow-up nursing home coverage and may have higher out-of-pocket expenses while in the hospital. Medicare pays hospitals more for admitted patients than observation patients. MORE from NPR and Kaiser Health News …
As HHS Moves To End Overload Of Medicare Claims Appeals, Beneficiaries Will Get Top Priority
By Susan Jaffe Jan. 21, 2014 KAISER HEALTH NEWS in collaboration with![]()
Medicare beneficiaries who have been waiting months and even years for a hearing on their appeals for coverage may soon get a break as their cases take top priority in an effort to remedy a massive backlog.
Nancy Griswold, the chief judge of the Office of Medicare Hearings and Appeals (OMHA), announced in a memo sent last month to more than 900 appellants and health care associations that her office has a backlog of nearly 357,000 claims. In response, she said the agency has suspended acting on new requests for hearings filed by hospitals, doctors, nursing homes and other health care providers, which make up nearly 90 percent of the cases. But beneficiaries’ appeals will continue to be processed.
“We have elderly or disabled Medicare clients waiting as long as two years for a hearing and nine months for a decision,” said Judith Stein, executive director of the Center for Medicare Advocacy. [More from KHN] [More from Washington Post]…
Link
HHS Inspector General Scrutinizes Medicare Rule For Observation Care
By July 30, 2013 | Kaiser Health News in collaboration with 
Medicare patients’; chances of being admitted to the hospital or kept for observation depend on what hospital they go to — even when their symptoms are the same, notes a federal watchdog agency in a report to be released today, which also urges Medicare officials to count those observation visits toward the three-inpatient-day minimum required for nursing home coverage.
The investigation, conducted by the Department of Health and Human Services Inspector General, was based on 2012 Medicare hospital charges. Its findings, which underscore several years of complaints that the distinction between an inpatient and observation stay isn’t always clear, come just days before the Centers for Medicare and Medicaid Services (CMS) is expected to issue final regulations intended to address the problem. [Continued in Washington Post and in KHN]
Link
Dan Driscoll used to be a smoker. During a regular doctor’s visit, his primary-care physician suggested that Driscoll be tested to see if he was at risk for an abdominal aortic aneurysm, a life-threatening condition that can be linked to  smoking. The doctor said Medicare would cover the procedure. So Driscoll, 68, who lives in Silver Spring, had the test done and was surprised when he got a bill from Medicare for $214.
smoking. The doctor said Medicare would cover the procedure. So Driscoll, 68, who lives in Silver Spring, had the test done and was surprised when he got a bill from Medicare for $214.
“I didn’t accept that,” he said, because based on everything he had read from Medicare, he was sure this was a covered service. So Driscoll did something that seniors rarely do: He filed an appeal. Of the 1.1 billion claims submitted to Medicare in 2010 for hospitalizations, nursing home care, doctor’s visits, tests and physical therapy, 117 million were denied. Of those, only 2 percent were appealed.
“People lose, and then they lose heart, or they are too sick, too tired or too old, and they give up,” said Margaret Murphy, associate director of the Center for Medicare Advocacy, which has offices in Washington and Connecticut. “Or their kids are handling the appeal and they are too overwhelmed caring for Mom or Dad.” [Continued at Kaiser Health News and The Washington Post.]
How To File A Medicare Appeal Here are some basic steps for challenging Medicare coverage denials…. [Continued at Kaiser Health News.]
