By Susan Jaffe KAISER HEALTH NEWS | July 7, 2015 | This KHN story also ran in 
Every month, a group of older adults goes to Washington’s Sibley Memorial Hospital, but they don’t see a doctor or get tests. They’re not sick. They come just for laughs.

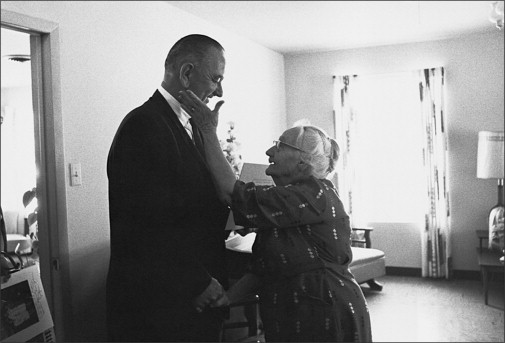
Joanne Philleo, 79, enjoys a joke at the monthly “Laugh Cafe” event at Sibley Memorial Hospital. (Amanda Voisard for The Washington Post)
They gather in a room next to the hospital cafeteria for the “Laugh Cafe,” one of the activities offered to local seniors, including the 7,300 members of Sibley’s Senior Association. The price of admission is one joke, recited out loud. Experts say laughing can be good for your health, and everyone in the room strongly agrees.
…The association for those age 50 or older also offers other activities, including French and Italian conversation classes, day trips to museums, a current events group, and — the latest addition — tango lessons. In addition, members receive discounts on hospital parking and at the gift shop, pharmacy and restaurant. In all, more than 10,000 seniors participate.
Sibley is one of several hospitals in the Washington area — along with others across the country — offering social activities and other benefits to help seniors stay healthy and out of the hospital, while encouraging them to visit. Participants do not need to have been patients.
But some experts are concerned that the activities are less about health than about marketing to Medicare beneficiaries, especially those who can go to the hospital of their choice when they need care because they are not enrolled in private insurance plans with limited provider networks.[Continued in Washington Post]…
![]()

 miss until patients are hit with big medical bills after a short stay.
miss until patients are hit with big medical bills after a short stay.
 antipsychotic drugs to staffing. Some are required by the Affordable Care Act and other recent federal laws, as well as the president’s executive order directing agencies to simplify regulations and minimize the costs of compliance.
antipsychotic drugs to staffing. Some are required by the Affordable Care Act and other recent federal laws, as well as the president’s executive order directing agencies to simplify regulations and minimize the costs of compliance. in a nursing home or long-term care facility, they need to know that their loved one’s health and safety are priorities.”
in a nursing home or long-term care facility, they need to know that their loved one’s health and safety are priorities.”


 Milford, population 2,100, Dr. Robert Wergin understands it’s not easy for some of his older patients to get to his office. Some may live on isolated farmsteads several miles out of town, and if they don’t drive, their son or daughter—if nearby—may have to take time off from work to bring them to their appointments because there’s no public transportation. Massive snowstorms are nothing special but still cause a wave of cancellations.
Milford, population 2,100, Dr. Robert Wergin understands it’s not easy for some of his older patients to get to his office. Some may live on isolated farmsteads several miles out of town, and if they don’t drive, their son or daughter—if nearby—may have to take time off from work to bring them to their appointments because there’s no public transportation. Massive snowstorms are nothing special but still cause a wave of cancellations. A disabled senior with serious health problems who successfully challenged Medicare for denying her home health care coverage has racked up another win against the government.
A disabled senior with serious health problems who successfully challenged Medicare for denying her home health care coverage has racked up another win against the government. charged a share of the cost. In addition to hospital bills, Medicare observation patients whose doctors order follow-up nursing home care will have to pay the nursing home themselves. Medicare covers nursing homes only after seniors are admitted to the hospital and stay through three consecutive midnights. A month in a Connecticut nursing home can cost as much as $15,000.
charged a share of the cost. In addition to hospital bills, Medicare observation patients whose doctors order follow-up nursing home care will have to pay the nursing home themselves. Medicare covers nursing homes only after seniors are admitted to the hospital and stay through three consecutive midnights. A month in a Connecticut nursing home can cost as much as $15,000. “It has been standard operating procedure that patients will be discontinued from therapy services because they are not improving,” she said.
“It has been standard operating procedure that patients will be discontinued from therapy services because they are not improving,” she said.

 hobbled with a meager budget and staffing, and it is facing a three-month deadline for its report. Speakers at the meeting reminded the commission that the effort is daunting.
hobbled with a meager budget and staffing, and it is facing a three-month deadline for its report. Speakers at the meeting reminded the commission that the effort is daunting. man Services Secretary Kathleen Sebelius. In January, a federal judge approved a settlement in which the government agreed that this “improvement standard” is not necessary to receive coverage.
man Services Secretary Kathleen Sebelius. In January, a federal judge approved a settlement in which the government agreed that this “improvement standard” is not necessary to receive coverage.